Filters
Host (768597)
Bovine (1090)Canine (20)Cat (408)Chicken (1642)Cod (2)Cow (333)Crab (15)Dog (524)Dolphin (2)Duck (13)E Coli (239129)Equine (7)Feline (1864)Ferret (306)Fish (125)Frog (55)Goat (36847)Guinea Pig (752)Hamster (1376)Horse (903)Insect (2053)Mammalian (512)Mice (6)Monkey (601)Mouse (96266)Pig (197)Porcine (70)Rabbit (358709)Rat (11723)Ray (55)Salamander (4)Salmon (15)Shark (3)Sheep (4247)Snake (4)Swine (301)Turkey (57)Whale (3)Yeast (5336)Zebrafish (3022)Isotype (156643)
IgA (13624)IgA1 (941)IgA2 (318)IgD (1949)IgE (5594)IgG (87187)IgG1 (16733)IgG2 (1329)IgG3 (2719)IgG4 (1689)IgM (22029)IgY (2531)Label (239340)
AF488 (2465)AF594 (662)AF647 (2324)ALEXA (11546)ALEXA FLUOR 350 (255)ALEXA FLUOR 405 (260)ALEXA FLUOR 488 (672)ALEXA FLUOR 532 (260)ALEXA FLUOR 555 (274)ALEXA FLUOR 568 (253)ALEXA FLUOR 594 (299)ALEXA FLUOR 633 (262)ALEXA FLUOR 647 (607)ALEXA FLUOR 660 (252)ALEXA FLUOR 680 (422)ALEXA FLUOR 700 (2)ALEXA FLUOR 750 (414)ALEXA FLUOR 790 (215)Alkaline Phosphatase (825)Allophycocyanin (32)ALP (387)AMCA (80)AP (1160)APC (15217)APC C750 (13)Apc Cy7 (1248)ATTO 390 (3)ATTO 488 (6)ATTO 550 (1)ATTO 594 (5)ATTO 647N (4)AVI (53)Beads (225)Beta Gal (2)BgG (1)BIMA (6)Biotin (27817)Biotinylated (1810)Blue (708)BSA (878)BTG (46)C Terminal (688)CF Blue (19)Colloidal (22)Conjugated (29246)Cy (163)Cy3 (390)Cy5 (2041)Cy5 5 (2469)Cy5 PE (1)Cy7 (3638)Dual (170)DY549 (3)DY649 (3)Dye (1)DyLight (1430)DyLight 405 (7)DyLight 488 (216)DyLight 549 (17)DyLight 594 (84)DyLight 649 (3)DyLight 650 (35)DyLight 680 (17)DyLight 800 (21)Fam (5)Fc Tag (8)FITC (30165)Flag (208)Fluorescent (146)GFP (563)GFP Tag (164)Glucose Oxidase (59)Gold (511)Green (580)GST (711)GST Tag (315)HA Tag (430)His (619)His Tag (492)Horseradish (550)HRP (12960)HSA (249)iFluor (16571)Isoform b (31)KLH (88)Luciferase (105)Magnetic (254)MBP (338)MBP Tag (87)Myc Tag (398)OC 515 (1)Orange (78)OVA (104)Pacific Blue (213)Particle (64)PE (33571)PerCP (8438)Peroxidase (1380)POD (11)Poly Hrp (92)Poly Hrp40 (13)Poly Hrp80 (3)Puro (32)Red (2440)RFP Tag (63)Rhodamine (607)RPE (910)S Tag (194)SCF (184)SPRD (351)Streptavidin (55)SureLight (77)T7 Tag (97)Tag (4710)Texas (1249)Texas Red (1231)Triple (10)TRITC (1401)TRX tag (87)Unconjugated (2110)Unlabeled (218)Yellow (84)Pathogen (489613)
Adenovirus (8665)AIV (315)Bordetella (25035)Borrelia (18281)Candida (17817)Chikungunya (638)Chlamydia (17650)CMV (121394)Coronavirus (5948)Coxsackie (854)Dengue (2868)EBV (1510)Echovirus (215)Enterovirus (677)Hantavirus (254)HAV (905)HBV (2095)HHV (873)HIV (7865)hMPV (300)HSV (2356)HTLV (634)Influenza (22132)Isolate (1208)KSHV (396)Lentivirus (3755)Lineage (3025)Lysate (127759)Marek (93)Measles (1163)Parainfluenza (1681)Poliovirus (3030)Poxvirus (74)Rabies (1519)Reovirus (527)Retrovirus (1069)Rhinovirus (507)Rotavirus (5346)RSV (1781)Rubella (1070)SIV (277)Strain (67790)Vaccinia (7233)VZV (666)WNV (363)Species (2982223)
Alligator (10)Bovine (159546)Canine (120648)Cat (13082)Chicken (113771)Cod (1)Cow (2030)Dog (12745)Dolphin (21)Duck (9567)Equine (2004)Feline (996)Ferret (259)Fish (12797)Frog (1)Goat (90451)Guinea Pig (87888)Hamster (36959)Horse (41226)Human (955186)Insect (653)Lemur (119)Lizard (24)Monkey (110914)Mouse (470743)Pig (26204)Porcine (131703)Rabbit (127597)Rat (347841)Ray (442)Salmon (348)Seal (8)Shark (29)Sheep (104984)Snake (12)Swine (511)Toad (4)Turkey (244)Turtle (75)Whale (45)Zebrafish (535)Technique (5597646)
Activation (170393)Activity (10733)Affinity (44631)Agarose (2604)Aggregation (199)Antigen (135358)Apoptosis (27447)Array (2022)Blocking (71767)Blood (8528)Blot (10966)ChiP (815)Chromatin (6286)Colorimetric (9913)Control (80065)Culture (3218)Cytometry (5481)Depletion (54)DNA (172449)Dot (233)EIA (1039)Electron (6275)Electrophoresis (254)Elispot (1294)Enzymes (52671)Exosome (4280)Extract (1090)Fab (2230)FACS (43)FC (80929)Flow (6666)Fluorometric (1407)Formalin (97)Frozen (2671)Functional (708)Gel (2484)HTS (136)IF (12906)IHC (16566)Immunoassay (1589)Immunofluorescence (4119)Immunohistochemistry (72)Immunoprecipitation (68)intracellular (5602)IP (2840)iPSC (259)Isotype (8791)Lateral (1585)Lenti (319416)Light (37250)Microarray (47)MicroRNA (4834)Microscopy (52)miRNA (88044)Monoclonal (516109)Multi (3844)Multiplex (302)Negative (4261)PAGE (2520)Panel (1520)Paraffin (2587)PBS (20270)PCR (9)Peptide (276160)PerCP (13759)Polyclonal (2762994)Positive (6335)Precipitation (61)Premix (130)Primers (3467)Probe (2627)Profile (229)Pure (7808)Purification (15)Purified (78305)Real Time (3042)Resin (2955)Reverse (2435)RIA (460)RNAi (17)Rox (1022)RT PCR (6608)Sample (2667)SDS (1527)Section (2895)Separation (86)Sequencing (122)Shift (22)siRNA (319447)Standard (42468)Sterile (10170)Strip (1863)Taq (2)Tip (1176)Tissue (42812)Tube (3306)Vitro (3577)Vivo (981)WB (2515)Western Blot (10683)Tissue (2015946)
Adenocarcinoma (1075)Adipose (3459)Adrenal (657)Adult (4883)Amniotic (65)Animal (2447)Aorta (436)Appendix (89)Array (2022)Ascites (4377)Bile Duct (20)Bladder (1672)Blood (8528)Bone (27330)Brain (31189)Breast (10917)Calvaria (28)Carcinoma (13493)cDNA (58547)Cell (413805)Cellular (9357)Cerebellum (700)Cervix (232)Child (1)Choroid (19)Colon (3911)Connective (3601)Contaminant (3)Control (80065)Cord (661)Corpus (148)Cortex (698)Dendritic (1849)Diseased (265)Donor (1360)Duct (861)Duodenum (643)Embryo (425)Embryonic (4583)Endometrium (463)Endothelium (1424)Epidermis (166)Epithelium (4221)Esophagus (716)Exosome (4280)Eye (2033)Female (475)Frozen (2671)Gallbladder (155)Genital (5)Gland (3436)Granulocyte (8981)Heart (6850)Hela (413)Hippocampus (325)Histiocytic (74)Ileum (201)Insect (4880)Intestine (1944)Isolate (1208)Jejunum (175)Kidney (8075)Langerhans (283)Leukemia (21541)Liver (17340)Lobe (835)Lung (6064)Lymph (1208)Lymphatic (639)lymphocyte (22572)Lymphoma (12782)Lysate (127759)Lysosome (2813)Macrophage (31794)Male (1617)Malignant (1465)Mammary (1985)Mantle (1042)Marrow (2210)Mastocytoma (3)Matched (11710)Medulla (156)Melanoma (15522)Membrane (105772)Metastatic (3574)Mitochondrial (160319)Muscle (37419)Myeloma (748)Myocardium (11)Nerve (6398)Neuronal (17028)Node (1206)Normal (9486)Omentum (10)Ovarian (2509)Ovary (1172)Pair (47185)Pancreas (2843)Panel (1520)Penis (64)Peripheral (1912)Pharynx (122)Pituitary (5411)Placenta (4038)Prostate (9423)Proximal (318)Rectum (316)Region (202210)Retina (956)Salivary (3119)Sarcoma (6946)Section (2895)Serum (24880)Set (167654)Skeletal (13628)Skin (1879)Smooth (7577)Spinal (424)Spleen (2292)Stem (8892)Stomach (925)Stroma (49)Subcutaneous (47)Testis (15393)Thalamus (127)Thoracic (60)Throat (40)Thymus (2986)Thyroid (14121)Tongue (140)Total (10135)Trachea (227)Transformed (175)Tubule (48)Tumor (76921)Umbilical (208)Ureter (73)Urinary (2466)Uterine (303)Uterus (414)From Zygote to Blastocyst: Stages of Embryonic Development In Vitro
Discover the fascinating journey of early human development in the lab. This post explores the stages of embryonic growth from fertilization to the blastocyst stage, highlighting key milestones observed during in vitro culture in IVF and research settings.
Genprice
Scientific Publications
From Zygote to Blastocyst: Stages of Embryonic Development In Vitro
Introduction
Fertilization occurs with the joining of the sperm and egg nuclei to create a new genetic program and a potential new individual. Until a little more than 20 years ago, the fallopian tube was the only place where a human could be conceived. Today, because of in vitro fertilization (IVF), this is no longer true. Since the birth of the first IVF baby in 1978, more than 1 million children have been born as a result of assistedreproductive technology (ART) procedures.All ART techniques involve manipulation of sperm and eggs to encourage fertilization and return of the resulting embryo(s) to the mother, where it is hoped that implantation and pregnancy will occur.
Although ART procedures can help many infertile couples, they challenge religious and social concepts of how parenthood is achieved.
Embryology Laboratories
Embryology laboratories have advanced significantly over the years. Today, the most successful labs follow strict protocols to ensure quality control and maintain a sterile, toxin-free environment. A range of specialized techniques has been developed to support fertilization, promote embryo development, and ensure accurate selection and safe transfer of embryos.
Fertilization
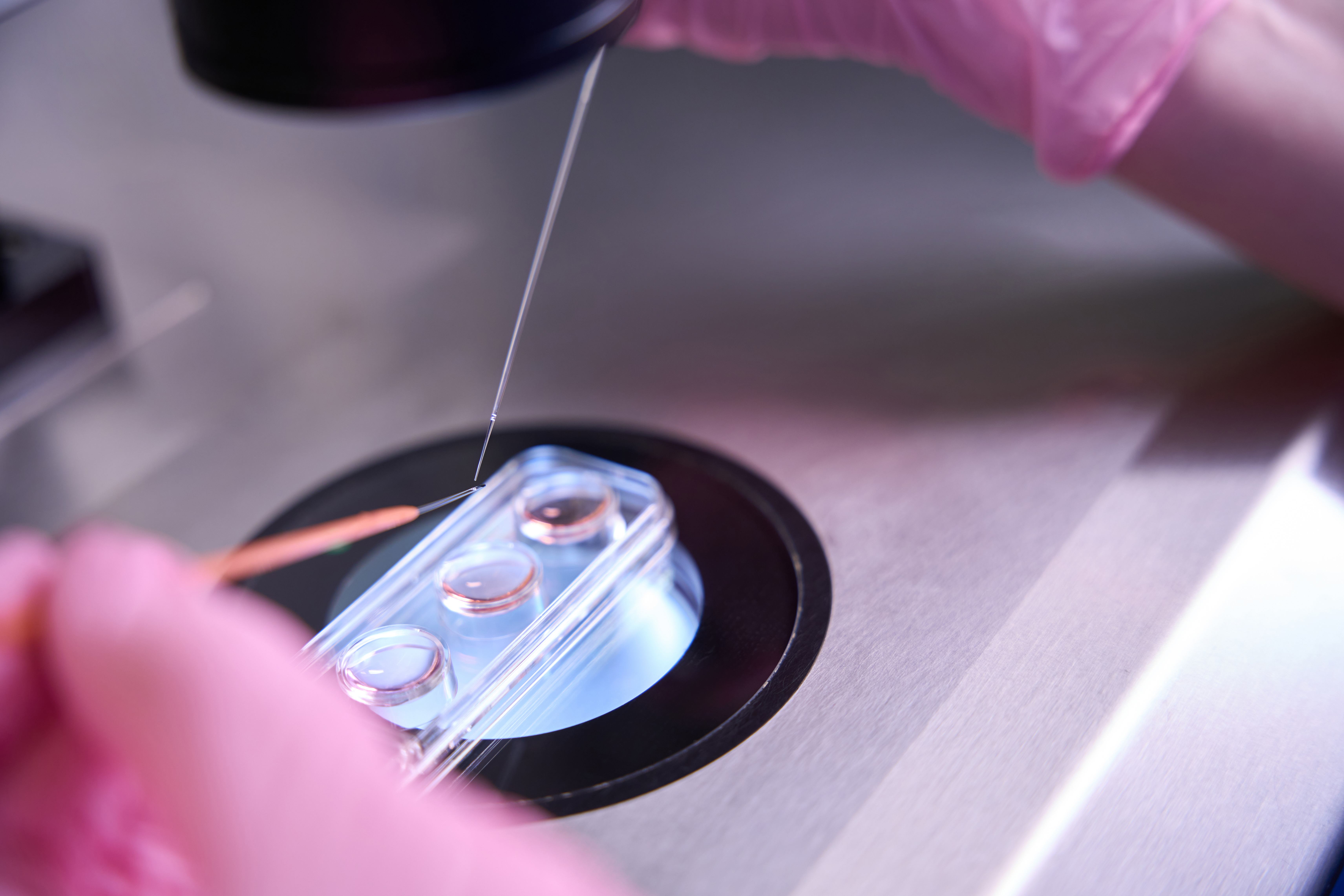
The expansion of assisted reproductive technologies (ART) to help couples with severe sperm abnormalities led to the development of micromanipulation techniques aimed at enhancing fertilization in the laboratory. Human eggs are surrounded by a protective layer called the zona pellucida, which sperm must penetrate to achieve fertilization. Early methods such as zona drilling and subzonal insertion were used to help sperm bypass this barrier and reach the oocyte membrane.
A major breakthrough came in 1992, when Dr. Gianpiero Palermo in Belgium successfully fertilized a human egg by directly injecting a single sperm cell into the cytoplasm of the egg—a technique now known as intracytoplasmic sperm injection (ICSI). At the time, many embryologists feared that bypassing the natural steps of fertilization might interfere with embryo development. However, Palermo demonstrated that ICSI could lead to the formation of healthy embryos and successful pregnancies.
The integration of ICSI into IVF has revolutionized the treatment of male infertility. Today, even a few viable sperm retrieved through testicular biopsy or epididymal aspiration can be used to fertilize oocytes, offering hope to couples who previously had few options beyond donor sperm or adoption.
Nevertheless, bypassing natural selection mechanisms raises important concerns. Men with genetic mutations or deletions affecting sperm production may pass these traits to their offspring. In some cases, such mutations are associated with other inherited conditions, such as cystic fibrosis. As a result, couples dealing with severe male factor infertility are strongly encouraged to undergo genetic counseling as part of their treatment planning.
Embryo Culture
During the initial five days post-fertilization, the embryo undergoes rapid development, transforming from a single-cell zygote into a multicellular blastocyst. A critical metabolic shift occurs during this period as the embryo transitions from relying on maternal genetic material to activating its own genome.
Standard embryo culture utilizes a basic medium composed of salts and nutrients, which supports the growth of high-quality embryos and yields good implantation and pregnancy rates. However, as the embryo develops, its metabolic requirements change. Sequential culture addresses this by employing different, more complex media formulations tailored to the specific developmental stage of the embryo, aiming to optimize its growth by meeting these evolving metabolic needs.
Embryo Transfer
Over the years, embryologists have significantly improved the ability to culture healthy embryos. In the 1980s, it was common to transfer six to eight embryos during a single procedure. Today, to reduce the risk of multiple pregnancies, most clinics transfer no more than two or three high-quality embryos. Embryo transfer typically takes place after three days of culture, although in some cases, culture may be extended to the blastocyst stage to allow for the transfer of a single, more developed embryo. If overall embryo quality is poor, more embryos may be transferred.
Embryos are transferred using a thin, flexible catheter, carefully guided through the cervix. The goal is to place the embryos in the mid-uterine cavity with a minimal volume of transfer medium. The procedure must be performed gently to avoid uterine bleeding, which could reduce the chances of implantation. For most patients, the transfer is painless.
Failures can occur if the embryos become trapped in cervical mucus or fail to exit the transfer catheter, but these issues are generally preventable with precise technique. Some clinicians use ultrasound guidance to ensure proper placement of the embryos inside the uterus.
A normal uterine cavity and receptive endometrium are key to successful implantation. Physicians often evaluate the uterine cavity before an ART cycle using hysterosalpingography or pelvic ultrasound. Endometrial polyps or submucosal fibroids are frequently removed beforehand to optimize the uterine environment. Following embryo transfer, progesterone supplementation is administered to support the development of a secretory endometrium.
Another technique used to improve implantation is assisted hatching. This involves making a small opening in the zona pellucida just before transfer, to help the embryo emerge and potentially enhance communication with the endometrium.
Conclusion
The journey from zygote to blastocyst represents a critical window in early human development one that has been closely studied and carefully supported in modern embryology laboratories. Thanks to decades of innovation in assisted reproductive technologies, fertilization and early embryonic growth can now take place outside the human body under controlled, optimized conditions. From precise sperm injection techniques to tailored culture media and careful embryo transfer protocols, each step plays a vital role in increasing the chances of successful implantation and pregnancy. As embryology continues to evolve, these advances not only offer hope to individuals and couples facing infertility but also deepen our understanding of human development at its very beginning.